Major technological, procedural, and pharmacological innovations in the past few decades have transformed the landscape of interventional cardiology, allowing procedures that once required over-night hospital stays to be performed in the outpatient setting [1]. The shift may cut costs and increase convenience for many patients. Procedures increasingly being performed in the outpatient setting include coronary and peripheral angiography/catheterization, coronary and peripheral angioplasty/stenting, and implantable cardioverter defibrillator (ICD) or pacemaker implantations. As the sizes of the incisions required for these procedures has decreased along with the risk of complications and/or bleeding, the need for overnight stays has likewise been reduced [1,2].
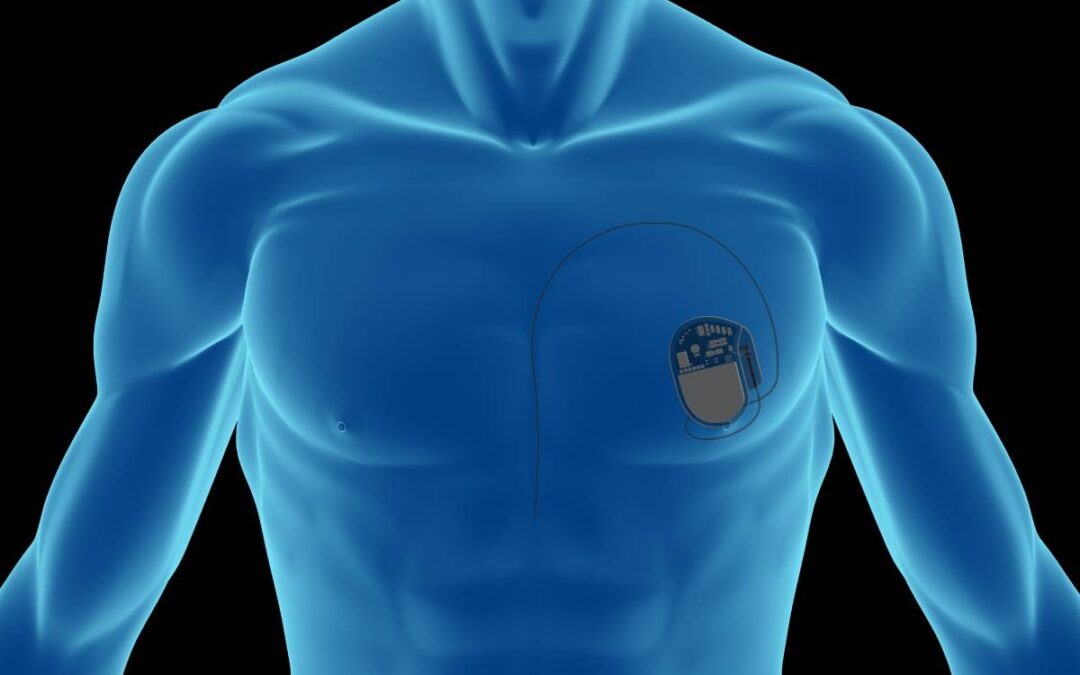
An example of a life-saving cardiac intervention that is being performed in the outpatient setting more frequently is the implantation of an ICD or pacemaker, devices that help manage arrhythmias and potentially lethal cardiac conduction disturbances. Since the first pacemaker was implanted by thoracotomy in the late 1950s, the procedure has evolved to be roughly one hour in length, most often utilizing transvenous implantation. This allows physicians to insert the pacing leads into a vein through a roughly two-inch incision and guide the device to the correct heart chamber with the aid of imaging technologies [3]. Studies have shown that same-day pacemaker and ICD implantations are safe [4]. Complications rates appear to be decreasing, with one study finding an in-hospital complication rate of 1.8% out of over 240,000 ICD implantations performed from 2010-2011 [5]. Further simplification of this procedure is likely, with the emergence of leadless pacing, which uses a smaller device, reduces risks of infection and complications from lead dislodgement or fracture, and does not require a chest incision [3].
The shift toward outpatient cardiology interventions will have a major financial impact on hospitals and payers. At one hospital in the UK, for example, same-day pacemaker implantations resulted in savings of roughly $34,000 between 2005-2006; in this study, only a minority of patients (109/780) were treated as outpatients, testifying to the greater expansion of outpatient care that is still possible.6 One study found that same-day dischargers for percutaneous coronary interventions (PCIs), which include coronary angioplasty/stenting and drug-eluting stenting procedures, are not only safe, but have the potential to save hospitals roughly $5,000 per case, due to reduced supply and room and board costs. If more same-day discharges for PCIs are used nationwide, the authors estimate US hospitals could save $577 million [7]. These savings should, ideally, be passed onto patients.
The ability to provide cardiovascular services in the outpatient setting may also shift revenue away from hospitals and toward ambulatory surgery centers (ASCs) [8]. Pacemaker procedures, along with peripheral vascular procedures, have historically been among the few cardiology services that the Centers for Medicare and Medicaid Services (CMS) has reimbursed when performed in the outpatient setting at ASCs, but this is changing. While roughly 10 percent of all cardiovascular (CV) procedures were performed in ASCs in 2018, CMS rule changes between 2019-2020 sanctioned reimbursement for over a dozen primary cardiac catheterization and coronary intervention procedures (including many PCIs) at ASCs [2,8]. If just five percent of PCIs shift to ASCs, CMS expects savings of $20 million in costs and $5 million in copays [1]. Since Medicare patients overwhelming represent those requiring the broad range of procedures now reimbursed in ASCs, a migration of just 10 to 30 percent of procedures could lead to a decrease of approximately $373 million to $1.1 billion in revenue for hospitals [8].
The American College of Cardiology (ACC) and the Society of Cardiovascular Angiography and Interventions (SCAI) have largely supported shifting some PCIs to the ASC with prudent risk stratification, safety measures, and proper reimbursement. In consensus statements published in 2014 and 2020 with the American Heart Association, they provide guidance for approving patients for ASC operations [2,8]. As the SCAI writes, ASC procedures offer “improved efficiency of care, increased access to care, better patient satisfaction, and reduced cost” [1]. And with bed-numbers of continued concern in the era of COVID-19, reducing unnecessary inpatient stays remains a primary consideration for health professionals [8]. The trend toward more and more cardiology procedures being performed on an outpatient basis may have significant benefits toward patients and may represent major changes in the healthcare landscape.
References
- Box LC, Blankenship JC, Henry TD, et al. SCAI position statement on the performance of percutaneous coronary intervention in ambulatory surgical centers. Catheter Cardiovasc Interv. 2020;96(4):862-870. doi:10.1002/ccd.28991
- Truesdell K, Griffith L. The Cardiovascular Shift to the Outpatient Setting. The Cardiovascular Learning Network. Published March 2022. https://www.hmpgloballearningnetwork.com/site/cathlab/cardiovascular-shift-outpatient-setting
- Beck H, Boden WE, Patibandla S, et al. 50th Anniversary of the first successful permanent pacemaker implantation in the United States: historical review and future directions. Am J Cardiol. 2010;106(6):810-818. doi:10.1016/j.amjcard.2010.04.043
- Rogstad TL, Powell AC, Song Y, et al. Determinants of outcomes following outpatient placement of implantable cardioverter defibrillators in a Medicare Advantage population. Clin Cardiol. 2018;41(9):1130-1135. doi:10.1002/clc.23041
- Dodson JA, Reynolds MR, Bao H, et al. Developing a risk model for in-hospital adverse events following implantable cardioverter-defibrillator implantation: a report from the NCDR (National Cardiovascular Data Registry). J Am Coll Cardiol. 2014;63(8):788-796. doi:10.1016/j.jacc.2013.09.079
- Osman F, Krishnamoorthy S, Nadir A, Mullin P, Morley-Davies A, Creamer J. Safety and cost-effectiveness of same day permanent pacemaker implantation. Am J Cardiol. 2010;106(3):383-385. doi:10.1016/j.amjcard.2010.03.038
- Amin AP, Pinto D, House JA, et al. Association of same-day discharge after elective percutaneous coronary intervention in the United States with costs and outcomes. JAMA Cardiol. 2018;3(11):1041-1049. doi:10.1001/jamacardio.2018.3029
- Kehayes N, Hartzell S, Reed K, Fisher N. Cardiac catheterization in the ASC – Strategic considerations for hospitals and health systems. Becker’s ASC Review. Published July 22, 2020. https://www.beckersasc.com/cardiology/cardiac-catheterization-in-the-asc-strategic-considerations-for-hospitals-and-health-systems.html




Recent Comments